Introduction
Grading trachoma
The WHO simplified grading system is a simple and reliable public health tool to identify populations with significant potentially blinding disease. It is not designed for the clinical assessment of individual patients with signs of trachoma less than those defined by WHO.
The Communicable Diseases Network of Australia1 recommends clinical grading of trachoma. The WHO simplified trachoma grading system is used by doctors, nurses and health practitioners who must be able to adequately, reliably and rapidly assess the signs of disease in everyone.
Note: In 2020 the WHO Grading System was revised.2 The definition of trachomatous trichiasis was amended to exclude trichiasis affecting only the lower eyelid.
| Grade | Signs | ||
|---|---|---|---|
|
Infectious
|
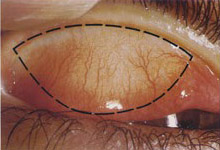
TF | Trachomatous inflammation – Follicular | Presence of 5 or more follicles of >0.5mm in diameter on the upper tarsal conjunctiva |
| TI | Trachomatous inflammation – Intense | Presence of pronounced inflammatory thickening of the upper tarsal conjunctiva obscuring more than half of the normal deep tarsal vessels | |
|
Non-infectious
|
TS | Trachomatous conjunctival Scarring | Presence of easily visible scars on the upper tarsal conjunctiva |
| TT | Trachomatous Trichiasis | Presence of at least one in-grown eyelash touching the eyeball, or evidence of recent removal of in-turned lashes | |
| CO | Corneal Opacity | Presence of corneal opacity blurring part of the pupil margin | |
The five signs are assessed independently. Each sign should only be included if it is easily visible.
The cornea and eyelids are examined first for evidence of in-turned eyelashes or corneal opacity.
Then the upper eyelid is everted, and the superior tarsal conjunctiva is examined for follicles, inflammation, and scarring. The examinations are done with 2.5× loupes and a good light source.





Laboratory tests
Trachoma as a public health problem in Australia is detected by clinical signs using the WHO simplified grading system.
Serology has been used to detect chlamydial infection in individuals. Researchers are exploring ways to use serology to help track trachoma endemicity but so far, the results are disappointing. More research is needed to determine if serology has any role to play.
Polymerase chain reaction (PCR) has been used for testing chlamydial eye infection. But it has some specific challenges. PCR has a high sensitivity. Specimens can easily be contaminated while taking swabs. Dead organisms can also give a positive PCR, so a positive test does not always mean the presence of viable or infectious organisms.
Only one quarter to one third of children who have TF will have PCR positive at any given time.3 About half the PCR positive tests in a community will be from children who have mild clinical signs of trachoma that are not severe enough to be graded TF.
1. CDNA 2014 National Guidelines for the Public Health Management of Trachoma [PDF]
2. Solomon AW, Kello AB, Bangert M, et al. The simplified trachoma grading system, amended. Bull World Health Organ. 2020;98(10):698–705. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7652564/
3. Michel CEC, Roper K, Divena M, Lee H, Taylor H. Correlation of clinical trachoma and infection in Aboriginal Communities. PLoS Negl Trop Dis. 2011; 5:e986 doi: 10.1371/journal.pntd.0000986